How to Normalize Stools and Restore Natural Bowel Movements
Moving bowels is an instinct, not an acquired trait. You don't need to teach newborns to move their bowels — it comes to them just as naturally as breathing or crying. Similarly, some seniors have never had a problem moving their bowels regularly and are free from common colorectal disorders, such as enlarged hemorrhoids, diverticular disease, or incontinence. So, why, then, so many other people aren't as lucky?
There are several noteworthy characteristics of these natural bowel movements that equally apply to happy babies, healthy seniors, and everyone in-between:
-
Strong defecation urge. Ideally, an intense sensation to move bowels is experienced after each principal meal, or at least once daily.
-
Small-sized stools. The stools are small, soft, and finger-sized, sometimes barely formed. By the Bristol Stool Scale classification, they correspond to type 4 to 6.
-
A small volume of stools. The weight of the stools is usually no more than 100-150 grams per bowel movement.
-
Unnoticeable act. The act of defecation is an effortless, quick, and complete passing of stools. It is no more noticeable than the act of urination. There is absolutely no conscious effort or straining.
If your bowel movements aren't as described above, it means they are no longer "natural," and you may be facing an elevated risk of major and minor colorectal disorders. They range from the ubiquitous hemorrhoids to colon cancer, and, in-between, just about anything else you can find under the Colorectal Diseases heading of any medical reference.
This guide will teach you how to restore natural bowel movements (assuming the damage you've already acquired hasn't gone too far), how to prevent new damages, and, above all, how to protect yourself from colon cancer.
Medical textbooks don't have a definition for a natural bowel movement, but there are plenty of terms which describe "unnatural" bowel movements. These are irregularity, costivity, large stools, hard stools, straining, incomplete emptying, constipation, and constipation-predominant IBS.
When patients seek help with any of the above conditions, medical doctors commonly translate all of them into two succinct terms — constipation or irregularity. For brevity, I'll use the term "constipation" throughout this guide instead of an awkward and lengthy "unnatural bowel movement," or an unspecific and tentative "irregularity."
Diarrhea is also an unnatural condition but on the opposite side of the spectrum. Because many aspects of this fast-moving disorder may require immediate medical intervention (particularly in children), its management, prevention, and treatment are entirely outside of this site's scope.
I was suffering while following my gastroenterologist's advice. He had me taking fiber supplements, and laxatives and still I was having a lot of bloating, pain, constipation and diarrhea. I thought I would eventually die of a ruptured bowel obstruction. I started your Hydro C and the Morning and Evening packs of vitamins and feel I have my wonderful life back. I don't have anymore pain or problems with constipation or diarrhea. Wow. I just want to say THANK YOU SO MUCH." K.B., Greendale, Wisconsin (via e-mail)
If anyone is crazy, it's definitely not you!
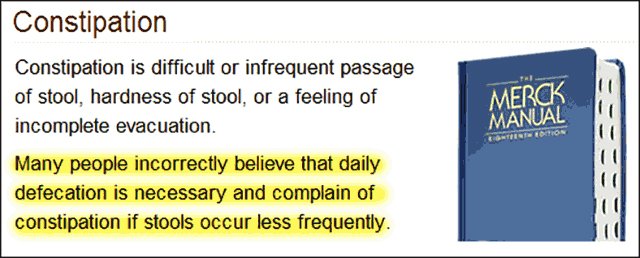
When doctors themselves seek guidance, they check out The Merck Manual of Diagnosis and Therapy, a highly influential and revered compendium of medical know-how. According to its publisher, it‘s "the world's most widely used medical textbook." Here is what the Constipation[1] section of the manual tells them (image modified to fit this page):
As you can see, according to Merck, unnatural bowel movements are perfectly acceptable. On the other hand, expecting a natural bowel movement is an "incorrect belief."
I don't know who the "experts" were who wrote this heresy, what sources they consulted while writing it, and who the editors were who let it get printed, but that's exactly what it says. Damn the endless body of human experience, damn academic knowledge, damn existing medical textbooks, and damn published research.
And the manual goes on to reinforce the dogma: "Physicians must explain that daily bowel movements are not essential…" And if patients ignore these recommendations, they are likely to be "obsessive-compulsive" and may get depressed "from the failure to defecate daily." Considering Merck's indisputable stature and authority, neither doctors nor patients are likely to question these recommendations.
As certain as rain in Georgia, a well-meaning doctor — already preconditioned to think that anyone complaining of constipation may be a psychotic crank — translates this asinine advice into comforting language, so the nutcase in front of him won't go postal:
— You have nothing to worry about, dear (...cranky bitch!..). It‘s probably in your head (...get a shrink, dummy!..).
— Thank you, doctor (...you, patronizing asshole!..). Thank you very much (...thanks for nothing, bastard!..). I‘ll try not to worry (...I need to find a better doctor...).
— You are very welcome, dear (...what an idiot...). And don‘t forget the fiber! See you soon. (...God, make her disappear...) Next patient, please!
This theater of the absurd plays day in, day out in medical offices everywhere. So it shouldn't surprise anyone to learn that constipation happens to be "the most common digestive complaint in the United States, outnumbering all other chronic digestive conditions [2]."
Here is what a genuinely knowledgeable and concerned doctor or nutritionist should have told you about restoring natural bowel movements, whatever your complaints and complications happen to be:
The
primer on fecal engineering
(Bowel movements demystified)
Ideally, dear, you should move your bowels every day, preferably after each major meal. Your stools are supposed to be small, light, and barely noticeable, just like when you were a baby and enjoyed completely natural bowel movements.
Constipation, irregularity, and hard stools have many causes. dysbacteriosis; the use of fiber to replace dead bacteria; the enlargement of internal hemorrhoids; an unfortunate tendency to withhold stools until the right bathroom is available; the use of laxatives; nerve damage related to medication, diabetes, or nutritional deficiencies; the fear of having pain or bleeding while moving bowels; the side effects of many commonly used medicines; and some others.
Your age, dear, doesn't affect natural bowel movements directly unless you've been experiencing problems for a long time, and your colon, rectum, and anus have already been irreversibly damaged by large stools. Obviously, the older you are, the more profound the damage. That's why people connect abnormal bowel movements with age.
If your colorectal organs are healthy, a regular diet doesn't play a significant role in natural bowel movements, even with a moderate amount of fiber, except for the dietary fat factor. Fat is essential to stimulate defecation. This diet-constipation connection is one of the most difficult to accept because people commonly equate food with stools.
Let me explain to you this food-stools connection in greater detail, otherwise you'll have a hard time restoring natural bowel movements or getting rid of constipation:
The largest component of stools is water — 65% to 85%. With low-fiber diets, undigested food remnants represent from 5% to 7% of total stool volume. With high-fiber diets, they represent 10% to 15%. That‘s why healthy people who fast or can‘t eat solid food because of a sudden medical emergency continue to move their bowels — food, as they say, doesn't make the weather.
This surprising disconnect between food and stools becomes self-evident after breaking down food staples into six essential components — water, carbohydrates, protein, fat, fiber, and ash. Only fiber is indigestible. The rest are digested either completely or almost completely:
-
Water from food and drinks is completely absorbed in the small and large intestine. Only about 100 ml (3 oz) of "embedded" water is excreted along with normal stools, but this is proportionately more in a high-fiber diet. Water content over 85% [3] — just a 10% difference — is characteristic of diarrhea.
-
Simple and complex carbohydrates (sugars and starches) digest completely in the small intestine (except lactose, which is fermented) and are absorbed into the blood as glucose, fructose, and galactose. More than 0.5% of undigested carbohydrates in the stools is considered abnormal [4].
-
Protein from meat, fish, fowl, dairy, seafood, and plants digests completely and is absorbed into blood as amino acids. So there‘s no protein in normal stools, except burned meat.
-
Close to 95% of all consumed fat is absorbed in the small intestine. Fat in stools above 6% [5] of consumed fat is considered abnormal. This condition is called steatorrhea.
-
All food contains insoluble mineral salts and the earth‘s minerals, which reach the large intestine undigested. This indigestible portion of food is called ash and is determined by cremation. Normal stools contain from 0.2% to 1.2% of ash.
Thus, if your daily menu includes 200 g of meats (2 g of ash), 100 g of fat (5 g undigested), and 200 g of digestible carbohydrates (1 g of ash), only 8 grams — one-and-a-half teaspoons — of undigested food residue will reach the large intestine. That‘s not enough to even get noticed in the toilet bowl.
The feces are kneaded into stools by intestinal peristalsis, with a generous serving of mucus secreted by the intestinal mucous membrane. The mucus binds together food residue, intestinal bacteria, and metabolic debris — dead body cells and remnants of metabolic activity shed by the liver along with bile.
After all is said and done, normal stools contain around 75% water. In other words, if you consume a low-fiber diet, your body expels 25 grams of undigested organic and inorganic matter for every 100 grams of stools, and only eight of those grams come from food.
The water in formed stools is retained by dead cells and intestinal bacteria, which are also single-cell organisms. Bacteria reside on the surface of the mucous membranes. They divide and die in huge numbers round-the-clock. The dead siblings are shed into the lumen (colon‘s cavity) and become an essential part of the stools. By some counts, dead bacteria represent up to 50% of dry stool matter, or almost 11 grams for each 100 grams of stools. (100 g – 75 g water – 5 g fats ) * 50% = 10 grams.
When bacteria are present, fiber has a moderate effect on the size and weight of stools because the bacteria ferment up to half of the insoluble fiber, while soluble fiber gets fermented completely. Thus, if your intestinal bacteria are alive and well, and you consume daily 20-30 grams of fiber from natural sources, it may add only 30 to 60 grams (the approximation of remaining unfermented fiber along with absorbed water) to the weight of your stools.
But if the intestinal bacteria are mostly dead (which is what causes constipation in the first place), and the dietary fiber remains unfermented, your stool weight will go up by 100-150 grams, because fiber attracts water up to five times its weight. The ensuing doubling of the stools‘ weight and size — the bulking up, conventionally speaking — will eventually cause the metamorphosis already described in all of the preceding guides.
According to Human Physiology by Schmidt and Thews — a textbook for medical students — people who consume fiber-rich diets excrete around 400 grams of stools daily. But that goes down to just 72 grams on a low-fiber diet, which is ideal! But with such a minuscule amount of normal stools, it‘s paramount not to miss bowel movements. Otherwise, small stools quickly dry out, become costive, and get difficult to pass out.
Keep in mind that the drying out of stools happens regardless of the bacteria count — normal stools become dry when the moisture content drops as little as 10% down to 65%.
When bacteria are missing altogether, the stools are dry from the get-go. That‘s why "fiber replacement therapy" works not just figuratively but literally — fiber retains water in place of the missing bacteria, though it isn‘t as efficient at keeping up the moisture as are bacterial cells. Remaining live bacteria keep devouring fiber and causing all of those prominent side effects of "rumination."
There is only one reliable way to prevent the drying up of stools and ensuing costivity — move your bowels after each big meal because the act of eating ALWAYS initiates the sequence of events that stimulate defecation. These successive unconscious events are called, respectively, the gastrocolic reflex, peristaltic mass movement, and the defecation urge. That‘s how our gut is wired by nature to move the bowels.
Unfortunately for most Westerners, once the potty training begins, the parents and teachers work really hard to unwire this miracle of nature. That‘s so that you can finally leave the house without a diaper and sit through a class without interrupting it. It‘s possible because the final stage of defecation doesn‘t take place until you consciously permit it by relaxing your external anal sphincter.
As we grow up, we learn to suppress the defecation urge by constricting our rectums with our pelvic muscles. While still young, we squint, grimace, and cross our legs to accomplish it; later in life, we can suppress all but the strongest urge, unnoticed and wrinkle-free.
But this essential social skill has a downside. If you keep suppressing defecation for too long, usually over a day, retained stools gradually impact, dry out, harden up, and require straining to get expelled regardless of size. When that happens, the chaffing of dry stools against the delicate lining of the anal canal causes big-time pain and scary-looking bleeding. (The straining makes matters much worse, as described here...)
To summarize, you should move your bowels as soon as you sense the defecation urge, usually after each big meal. In this ideal situation, stools are soft, small, and barely formed, which is perfectly normal. They weigh no more than 100-150 grams.
If this optimal frequency isn‘t attainable, you should pass stools at least daily, usually after breakfast. In this case, the stools accumulated over a 24-hour are larger, heavier, and more formed, but still passable.
On the other hand, when:
-
Your stools are larger than your middle or index finger, or… [These two sections — How Large Is To Large and The Final Frontier Between You And the Toilet Bowl — explains the connection between the size of stools and chronic constipation, a very important read]
-
Your stools weigh substantially more than two standard-issue ballpark wieners, or…
-
You need to strain, or you are experiencing discomfort, or…
-
You don‘t have effortless stools at least daily, or…
-
You are supplementing with fiber, or rely on prune juice, oatmeal, and/or laxatives...
…or all of the above, this truly means that something is wrong. Nonetheless, you aren't considered constipated until you don't move the bowels for more than three consecutive days. Thus, as long as you can keep straining to squeeze out stale, stinking, chaffing stools every three days, then, medically speaking, you are just irregular or not yet worse enough to warrant medical treatment. That's the essence of it.
— Thank you, doctor, this was a great explanation. I am beginning to understand now. But I am still not clear on how to get rid of constipation?
— Unfortunately, dear, there are no drugs or treatments that I can prescribe to you. And you are better off not using fiber or laxatives.
— So what should I do, then, doctor?
— I would love to help you more, but our appointment is already 30 minutes too long. Your insurance company isn't paying me a penny for talking 'crap', and I have other patients waiting. There is this medical writer in New Jersey, whose name is Constantine-something, and he wrote a GutSense.org web site. That's where I learned these things I just told you. Read his site. Find what applies to you, and follow it. You will not suffer from constipation ever again! I am embarrassed to admit it, but it helped me too! This guy is a genius.
— But what about The Merck Manual, doctor? The printout I brought is the complete opposite of what you just told me.
— Oh, forget about this rubbish, dear... It's a pharmaceutical company, for laughing out loud! They peddle Miralax, for heaven's sake... From their perspective, if you are complaining about constipation, you are a nutcase! Would you like me to send you to a psychiatrist, dear? I hope not...
— Thank you, doctor! Thank you very much! I am so lucky to know you! And I mean it... (...crying...)
— See you soon, dear. Don't cry, you‘ll be fine now... Just get rid of that fiber!.. Don't strain!.. It's g-u-t-s-e-n-s-e-dot-com. (...God, I lost another patient... She is so cute... Oh, well...) Next patient, please!
The trouble you went through in compiling this page helped a person on the other side of the world. And this I cannot thank you enough for. I appreciate the fact that you did not try and sell this information but made the first priority helping others. The world could use more people like you.
This is just my honest gratification letter, I appreciate your website very very much! Thank you. J.S., South Africa (via e-mail)
Bad advice: the harder they try — the faster you die...
That was, as I said, a best-case scenario. In real life, even if you meet a friendly, caring doctor who won't take you for an obsessive-compulsive psycho and who will go out of his/her way to help you, the primary recommendations would still boil down to the following well-known list:
(1) Consume 20 to 30 grams of fiber daily to ensure adequate stool bulk;
(2) Drink at least eight glasses of water daily to keep stools moist;
(3) Exclude animal fat because it causes constipation;
(4) Exercise regularly to stimulate intestinal activity;
(5) Tone up lax abdominal muscles because they improve elimination;
(6) Reduce stress because it contributes to constipation.
Too bad none of these recommendations are even remotely helpful for restoring natural bowel movements! And some are downright harmful. So, let's go over them one by one:
Q. Is it true that dietary fiber prevents or relieves constipation?
Q. Is it true that drinking more water prevents or relieves constipation?
Q. Is it true that regular exercise stimulates intestinal activity?
Q. Is it true that toning up lax muscles helps to relieve constipation?
Q. Is it true that dietary fiber prevents or relieves constipation?
No, it isn‘t. As I already explained in my book, here, and pretty much elsewhere on this site, fiber from fruits, vegetables, grains, bran, and laxatives is the PRIMARY cause of chronic, persistent constipation and related colorectal disorders.
For those who are familiar with the large intestine‘s anatomy, it isn't difficult to comprehend why fiber‘s most heralded asset — its ability to bulk up stools — is complete nonsense. The fiber‘s journey inside the large intestine begins not by going down, but by going up, up, and up the ascending colon. And the weightier it is, the longer it takes because the peristaltic propulsion inside the colon isn‘t strong enough to move up very heavy 'loads.'
This also explains how astronauts who spend months on end in the International Space Stations don‘t experience constipation, even though their stools are WEIGHTLESS. And when they do, they don‘t use fiber, but conventional laxatives, such as Ducolax® or Senade [6].
I do not understand this, but I had regular bowel movements when consuming NO fiber whatsoever. And yet when I consume ZERO fiber, getting all my calories from fiber-free foods, I have bowel movements 2x or more a day. I have lived on dairy products for weeks at a time, experienced two or more bowel movements a day, and never had any encounter with dietary fiber. Thank you so much for opening my eyes. P.D., USA (via e-mail)
Q. Is it true that drinking more water prevents or relieves constipation?
No, it isn‘t. Actually, sipping two, three, five, ten or more liters of water wouldn‘t produce soft and moist stools because drinking water per se never reaches the large intestine of a healthy person. In fact, death from water intoxication would happen faster than this water reaching the bowels.
For starters, the gastrointestinal tract isn‘t a straight pipe. Next, water gets absorbed in the small intestine long before it reaches the large intestine. In case it doesn‘t, you get hit with diarrhea. It only happens when inflammation, soluble fiber, or laxatives cause intestinal malabsorption.
Next, the large intestine excretes about 100-150 ml of water a day along with normal stools. That‘s around six-nine tablespoons of water from about 30 to 40 liters (8 to 10 gallons) present in the adult body at any time — more than enough to keep stools moist long after you die from dehydration.
Even more facts: According to Karl Fischer‘s [7] method of measuring the water content of feces, the difference in water content between hard, formed, grayish stools (that‘s as bad as it gets) and normal stool is less than 15 ml — a tablespoon‘s worth. In other words, you don‘t need to drink two liters of water to make up for one tablespoon.
Finally, the large intestine recovers sodium chloride — table salt in plain English — back from stools. Salt is needed body-wide to keep blood adequately salty, prevent edema, avoid dehydration, make sweat, and synthesize hydrochloric acid for gastric digestion. If you don't consume enough salt, stools get dehydrated even faster thanks to the intense recovery of sodium chloride from the large intestine.
It‘s worth noting that regular table salt is also the primary source of dietary iodine in the American diet. Iodine is required for a healthy thyroid function. Hypothyroidism happens to be one of the major causes of persistent, chronic constipation.
Incidentally, a low-salt diet lowers blood pressure not because salt causes it (salt consumed in moderation doesn‘t, the idea that it does is another big lie, waiting to get debunked), but because, at least initially, sodium deficiency causes dehydration. In turn, this reduces the volume of blood. Less blood in the system = less blood pressure. That‘s a no-brainer.
Later on, the low thyroid function kicks in and slows down the metabolism. Slow metabolism, in turn, reduces heart output and muscle tone. Along with hypotension (low blood pressure), these are the top reasons behind chronic fatigue in general, and "colon fatigue" (a.k.a. lazy gut) in our particular case.
If you are still in denial over eight glasses of water, the arch-conservative Journal of the American Dietetic Association nods in agreement with some of these points:
"It is a common but erroneous belief that the increased weight [of stool] is due primarily to water. The moisture content of human stool is 70% to 75% and this doesn‘t change when more fiber is consumed. In other words, fiber in colon is not more effective at holding water in the lumen than the other components of stool [8]."
If there is a connection between water consumption and constipation, it‘s the complete opposite: the more water you consume, the drier the stool gets because the excess water consumption causes the depletion of sodium chloride (table salt). Salt happens to be one of the most critical factors responsible for water retention in the stools. This very pervasive fiber-water myth is discussed in Chapter 2, Water Damage.
And, by the way, all that calcium and magnesium that your heart, teeth, joints, and bones are craving 24/7 gets pissed away as well. The more you drink, the faster...
End of story.
Out of desperation, I looked to research to find out why my seemingly healthy 13 year old daughter (who drank no milk products, no junk food, and minimal processed foods) could eventually lose all control of her bowels. It didn't take me long to eventually find your website. She is now cured (so far so good after one month). I am currently working on making you famous in my home town. J.L. Canada (via e-mail)
Q. Is it true that regular exercise stimulates intestinal activity?
No, it isn‘t. In fact, you can exercise yourself senseless and get even more constipated because, among other things, vigorous physical activity inhibits motility — a fancy term for forward propulsion of stools inside the large intestine. Reconfirmed by checking up Rome II:
"Active or chronic [sic] physical exercise has probably no major effect on the functions of healthy colons. [ 9 ] "
Besides, most people move their bowels for the first time just after waking up and having breakfast. A good night‘s sleep is hardly 'exercise.'
That erroneous concept came from correctly noting that fit and healthy people complain of constipation less often than sedentary types. But that concomitance (more exercise — less constipation) is an outcome of good health habits, not exercise. If there were a connection, constipation simply wouldn‘t exist among athletes, laborers, gym-goers, and beach jocks and bunnies. But of course, that isn‘t remotely the case. It doesn‘t mean that you shouldn‘t exercise. You absolutely should for all the other benefits it gives you.
There are several good reasons behind morning stools. First, while you are asleep horizontally, the large intestine propels feces toward the rectum. The propulsion up the ascending colon in the upright position is quite limited. Second, you are relaxed and not yet constrained by clothing. Third, eating breakfast stimulates the defecation urge. Finally, because you may be more comfortable using your own bathroom, you are less likely to suppress the defecation urge and will take immediate advantage of all of the above circumstances.
If you don‘t eat breakfast at home, you may stimulate defecation by slowly drinking a glass of warm water. This simple method is often as good a stimulant as eating. If you don‘t experience any urge, you may have anorectal nerve damage caused by fiber, straining, hemorrhoids, scarring, enlarged colon, medications, laxatives, diabetes, vitamin deficiencies, surgeries, and other factors described here.
Q. Is it true that toning up lax muscles helps to relieve constipation?
No, it isn‘t. Actually, stronger pelvic and abdominal muscles only help you to strain harder, and straining aggravates constipation and its side effects more than any other single factor. And that‘s before considering the impact of straining on hemorrhoids, rectal prolapse, hernias, diverticular disease, intestinal obstructions, genitourinary disorders, and other possible complications. As I already explained, normal defecation requires no more abdominal "push" than urination. It ain‘t childbirth, dahlings…
If you still keep straining after reading this, consider taking a Lamaze class to reduce pain and anxiety. Just imagine the helping hand and reassuring voice of your beloved spouse guiding you along: exhale darling, push, push, push, poop… You are doing great!… Inhale, relax, relax, relax… OK, let‘s do it again!
Please note again that I am not against having toned and beautiful "six-pack abs" per se, but against using them to "relieve constipation." A small but significant difference.
Q. Is it true that stress causes constipation?
Yes and no, depending on personality type, circumstances, and stress severity.
Yes, because depression and anxiety inhibit gastric and intestinal peristalsis and sometimes result to conscious suppression of bowel movements. Additional culprits are the medicines taken for anxiety, depression, and insomnia — along with a runaway mind, drugs dull the nerves and muscles vested with elimination duties all too well.
No, because intense stress may cause the complete opposite of constipation: diarrhea of equal intensity. Hadn‘t you ever experienced a nasty churning inside your gut while facing a first date, or crucial exam, or job interview, or speed trap, or close call, or IRS audit, or… perhaps even from reading this article?
I discuss the connection between stress and constipation at length on this page: Does Stress Cause Constipation And Why?
Q. Is it true that animal fat causes constipation?
No, it isn‘t. In fact, it‘s the complete opposite: low-fat diets cause constipation, while excess fat causes diarrhea. Anyone who tells you otherwise needs a mental check considering that vegetable oils have been used as potent laxatives for millennia. Chemically, flax, olive, or castor oils are fat just as much as lard, tallow, or butter — except they are liquid and easier to swallow in one large dose.
Any fat taken at once in large quantities as a "purgative" overwhelms the intestinal fat-breaking enzymes and remains largely undigested. This condition blocks the absorption of fluids throughout the entire length of the small and large intestines and causes a surge of fluids straight down into the rectum. The large volume of fluid inside the rectum causes diarrhea, just like an enema does. That‘s all there is to it.
Is this a safe fix for persistent constipation? No, it is neither safe nor effective. First, you may end up dehydrated because fluids can‘t be absorbed. Second, oil-based laxatives cause soiling or persistent fecal incontinence. Third, vegetable oils may contain carcinogenic trans fats, plant-derived toxins, and allergic irritants that may cause intestinal inflammation. Fourth, mineral oil (it‘s indigestible, but still gets absorbed into the blood) may cause severe poisoning and lipid pneumonia.
Adding insult to injury, oil-based laxatives are impractical for severe constipation because oil coats up hardened stools and prevents surging fluids from breaking them down. The resulting diarrhea is called paradoxical, because fluids flow around stools, while they remain stubbornly lodged inside the large intestine.
Finally, why do low-fat diets contribute to constipation? Dietary fat stimulates the release of bile from the gallbladder, which, in turn, stimulates the gastrocolic reflex. This, in turn, stimulates peristaltic mass movement, which, in turn, stimulates defecation. No fat in the diet = not enough bile in the system to get the ball rolling:
"Energy-rich meals with a high-fat content increase motility [propulsion of stools]; carbohydrates and proteins have no effect." (Source: Human Physiology [10])
Case closed!
Apparently, that harebrained conjecture about animal fats and constipation came from observing the Atkins diet's costivity effect. But this fluke has nothing to do with fat and everything to do with fiber — or, more accurately, with the absence of fiber in low-carb diets. Naturally, stools sans fiber lack the bulk to get coaxed out on their own from a large intestine damaged by years and years of fiber dependence.
I‘ve lavished extra attention on the fat-constipation connection because anything remotely related to fat, and, indirectly, to cholesterol, is so controversial.
Talking of cholesterol… Every single cell in your body is covered by membranes made from the molecules of cholesterol. The intestines happen to be one of the most demanding consumers of cholesterol because all of the cells that make up intestinal membranes get turned over (replaced) daily. The cholesterol needed to make up these cells comes from food or is synthesized by the liver as LDL ("bad") cholesterol. Whenever you restrict food sources of cholesterol, your liver has to produce more LDL cholesterol to compensate for the deficit.
On the other hand, HDL ("good") cholesterol is the principal component of bile. The more fat you ingest, the more bile is made by the liver to digest it, and, correspondingly, the level of HDL cholesterol goes up.
Thus, if you limit dietary fat and cholesterol, the "bad" goes up to kill you, and the "good" goes down to kill you more. On the other hand, with its plentitude of animal fat and cholesterol, the Atkins diet has been consistently shown to lower the "bad" and raise the "good" cholesterol — just what the doctor ordered.
This phenomenon — less animal fat, more "bad" cholesterol — hasn‘t, of course, escaped the attention of statin-makers (LDL-lowering drugs such as Lipitor, Zocor, Crestor, Mevacor, Pravachol, Vytorin, etc.). No wonder they promote low-fat diets with the vengeance of John McClane — the less animal fat you consume, the higher the LDL. And that sells more statins.
At this point, it shouldn‘t surprise you that constipation and diarrhea are listed among the most common side effects of statins [11]. Oh, well…
THANK YOU for your book and your website! They saved my life. I called my doctor Monday and canceled my colonoscopy that was scheduled for today. I am responding to the techniques described in your book. I have had years of distress - you can imagine. Anyway, it is a miracle... P.S., USA (via e-mail)
Recommendations: no downside, just upside-down
For starters, let‘s not pile up any more damage. Exercise for health, fun, and weight-loss reasons, but exercise doesn't stimulate intestinal activity — it inhibits it. If your colon is stuffed with week-old stools, then exercises that engage abdominal muscles may have a stimulating effect. But that's similar to straining and has nothing to do with normal defecation.
It's also perfectly OK to tone up lax abdominal muscles to improve your body shape, but don't use these muscles to squeeze out stools—unless you have a death wish! By all means, reduce stress in your life because stress hormones affect your cardiovascular system, your mood, your sleep, your appetite, and so on. But it makes no significant difference for constipation. In fact, an occasional jolt of stress is a very effective laxative.
Now, let's get down to the business of restoring natural bowel movements:
Step 1. Reduce fiber consumption and break any dependence on laxatives to the absolute minimum as described throughout this site, and particularly here. It's best if you read Fiber Menace — its last three chapters deal exclusively with a trouble-free transition to a low-fiber lifestyle. This step is essential to reduce stool size and restore proper (physiological) stool morphology.
Step 2. Reduce water consumption, as described in Chapter 2 of Fiber Menace: Water Damage. This step is important, particularly if you already have upper digestive disorders or are over 40, because overconsumption of water causes indigestion, gastritis, enteritis, and, surprisingly, dehydration related to the loss of essential electrolytes with excessive urination. This condition that may contribute to the onset of dehydration. You are better off avoiding and preventing all these conditions to avoid their cascading influence on constipation.
Step 3. Get off fat-free diets. Fat is the single most crucial factor in the physiology of defecation as we have already established above. Fat is also critical for normal digestion, a healthy GI tract, vitamin absorption, heart and brain function, blood cells, hormones, supple bones, and, of course, to overcome constipation. You can learn more about it here.
Step 4. Normalize stools. Use Hydro-CM program to attain small stools. The goal is to eliminate straining, reduce pressure on internal hemorrhoids, and restore anorectal sensitivity. If you are still relatively young and "undamaged," you should be able to restore natural bowel movements within a few weeks to a few months.
Step 5. Restore your intestinal flora. This step is executed in parallel with Step 4. An in-depth background about the role and function of intestinal flora is available here.
Step 6. Restore/awaken your anorectal sensitivity. Without this, you'll never feel the urge to move your bowels and won't be able to initiate unassisted, regular bowel movements. Even when the anorectal sensitivity is beyond repair, there are "ways and means" to attain desired results. More on this subject is here.
And that's all there is to it — a ton of fun reading, several inexpensive supplements, some bowel re-training, and "they moved their bowels happily ever after." Good luck!
With months of feedback using your principles, let me tell you that my condition has dramatically improved. It's not a perfect science. I jungle with pro/prebiotics, glutamine, minerals, vitamins, and, most of all, C ascorbate flushes when needed. Although not wholly cured, I'm not anymore at the mercy of endless problems.
Maybe most important of all, the dramatic reduction of my fiber consumption, dramatically reduced gastrointestinal crisis and instability of my guts.
I see myself so often asking people to think about the fibers they ingest like cows when they complain of GI troubles. You are certainly RIGHT about your principles, and the vision I have on food and guts is forever changed. The world needs to know." B.M., USA (via e-mail)
Frequently Asked Questions
Q. Why do women get constipated more often than men?
Q. What is the difference between irregularity and constipation?
Q. Is constipation dangerous for my health?
Q. How often should I move my bowels?
Q. Why do some foods cause constipation?
Q. Does stress cause constipation, and why?
Q. Does alcohol cause constipation?
Q. Why does anal sex cause constipation?
Q. What causes the traveler's constipation?
Q. Why is my infant constipated?
Q. Why is my toddler suddenly constipated?
Q. What are the causes of constipation in older children?
Q. What is the connection between autism, infant constipation, and diarrhea?
Q. What is the connection between constipation and the epidemic of juvenile diabetes?
Q. Why do doctors recommend fiber to treat constipation?
Q. Why doctors aren't recommending a recovery protocol similar to your Hydro-CM program?
Q. Is it true that dietary fiber prevents or relieves constipation?
Q. Can I relieve constipation by drinking more water?
Q. Is it true that regular exercise stimulates intestinal activity?
Q. Is it true that toning up lax muscles helps to relieve constipation?
Q. Is it true that animal fat causes constipation?
Q. Why do Atkins-style diets (i.e., low-carbohydrate) cause constipation?
Q. What is the best diet for constipation relief?
Q. Why do antibiotics cause constipation?
Q. Does smoking cause constipation?
Q. Why does colonoscopy cause constipation?
Q. Why does surgery cause constipation?
Q. Why does hot weather cause constipation?
Q. Can constipation cause acne?
Q. What are the causes of constipation during pregnancy?
Q. Why does constipation cause enlarged internal hemorrhoids?
Q. Why does constipation cause anal bleeding?
Q. Why does constipation cause bloating and flatulence?
Q. Why does constipation cause chronic fatigue?
Q. Can constipation reduce my immunity?
Q. Can constipation cause bad mouth odor?
Q. Is it true that old stools can cause “encrustation” of the large intestine's walls?
Q. What is the connection between constipation and appendicitis?
Q. What is the connection between constipation and colorectal cancer?
Q. What are the most common side-effects of traditional laxatives?
A. What is the connection between constipation and the epidemic of juvenile diabetes?
The pancreatic duct terminates in the duodenum, the first section of the small intestine that comes right after the stomach. The duodenum is particularly small in young children and can be easily obstructed by the fiber in morning cereals, fruits, vegetables, or supplements, mainly when provided to relieve constipation. The ensuing obstruction, even brief, may block the pancreatic duct and cause inflammation of the pancreas. In turn, acute pancreatitis may destroy the insulin-producing beta cells in the islets of Langerhans. A child without functional insulin-producing cells is condemned to a life of blood sugar monitoring, insulin injections, and all that follows. By age 40, the mortality rate among children affected by type I diabetes is twenty times higher than in the general population. I discuss the likely events preceding pancreatitis here.
A. Why do Atkins-style diets (i.e., low-carbohydrates) cause constipation?
Fiber is derived from plants (fruits, vegetables, grains) and plant-based processed foods, such as cereals, bread, and pasta. Plants and plant-based food happen to be a primary source of carbohydrate in the diet. Thus, any diet that is low in carbohydrates is also low in fiber, leading to a rapid reduction in stool size and weight.
If a person isn't dependent on fiber to move the bowels, this reduction of size and weight improves regularity and eases bowel movements. On the other hand, if fiber dependence is already present — a condition manifested as latent constipation — regular bowel movements are disrupted because the "plunging" effect of the fiber-heavy stools has gone.
In general terms, if you experience constipation after a sudden reduction of fiber in your diet, it means that you are already affected by a range of bowel disorders of different severity, such as dysbacteriosis, enlarged internal hemorrhoids, enlarged colon and rectum, and anorectal nerve damage.
To address fiber dependence, please review this page: Overcoming Fiber Dependence.
A. What is the best diet for constipation relief?
The best diet to prevent constipation is a diet low in fiber to maintain small and light stools, and moderate in fat to stimulate the moving of the bowels. Dietary fat is the only substance that initiates the action that precedes bowel movements. You can learn more about the role of fat in the physiology of the bowel movement on this page: Why Do Some Foods Cause Constipation?
For the record, I am not endorsing or recommending high-fat diets along the lines of Dr. Atkins. Just like high-carbs, high-fat diets contribute to obesity, hypertension, and heart disease because 95% to 98% of all fats get digested, and fat carries 225% of the energy content of carbohydrates. Besides, practically all processed vegetable fats are toxic and potentially carcinogenic to humans.
I am also not endorsing or recommending low-fat diets along the lines of Dr. Ornish. Low-fat diets of any kind cause severe digestive and metabolic disorders and contribute to cardiovascular disease, hypertension, depression, cancers, infertility, osteoporosis, osteoarthritis, periodontal disease, tooth loss, premature aging, and a host of other degenerative disorders.
I recommend a diet moderate in animal fat along the lines of the USDA Daily Recommended Allowances (DRA) of about 1 g of fat per 1 kg of body weight. This amount should be increased for growing children, underweight, pregnant women, seniors, people recovering from a disease, and similar circumstances. I describe the reasons behind these recommendations on this page: The Ingredients of Longevity Nutrition.
A. Why do antibiotics cause constipation?
Antibiotics are broad-spectrum antibacterial medicines expressly used to kill pathogenic bacteria throughout the body. With few exceptions, antibiotics can't differentiate good bacteria from bad, so all get killed, including the bacteria in the large intestine that give stools their amorphous properties — slightly formed, light, uniform in color, soft, and moist.
Once the bacteria population is reduced, or it is missing altogether, stools become dry and hard (type 1 on BSF scale) because there is nothing left to form them and to retain moisture. I describe the role of intestinal flora on this page: Dysbacteriosis (Dysbiosis).
The pathologies related to missing bacteria — constipation, low immunity, the deficiency of biotin and vitamin K, mucosal inflammation — are further exacerbated by medical doctors, particularly in the United States, who recommend using indigestible fiber to bulk up the stools instead of restoring the population of innate bacteria killed by antibiotics.
A. Does smoking cause constipation?
No, not really... Smoking stimulates moving the bowels because the continuous swallowing of the nicotine-laced saliva stimulates the gastrocolic reflex — an involuntary condition that initiates bowel movements.
Also, the smoke itself increases the level of CO2 in the blood. The ensuing vasodilation (widening) of the blood vessels helps intestinal peristalsis and amplifies the urge to move the bowels.
For the same reason smoking reduces the risks of constipation, smoking cessation is commonly associated with the onset of chronic constipation — the reduced stimulation diminishes the frequency and urgency of bowel movements, enlarges stools, and precipitates costivity, irregularity, straining, and fiber dependence — all of the hallmarks of latent and organic constipation.
If you are quitting smoking, you should pay particular attention to the risk of constipation and it's prevention, but without getting hooked on fiber and/or laxatives. Study the rest of this site to proactively identify the type and stage of your constipation to select the best treatment and preventative approach.
A. Why does colonoscopy cause constipation?
Colonoscopy procedure disrupts natural bowel movements. The four principal causes are (1) Intestinal flora damage by synthetic laxatives; (2) complete lavage of the bowels; (3) the side effects of anesthesia, and (4) stress and anxiety related to cancer screening.
If you are already affected by latent or organic constipation, resuming regular bowel movements is even more difficult. You can find a great deal more information on these side effects of colonoscopy on this page: Side Effects of Screening Colonoscopies.
Use all or some of the components of the the Hydro-CM program to restore regularity and to prevent further damage. To prevent kidney damage, severe dehydration, and blood clotting related to traditional colonoscopy prep as well as to spare intestinal flora from damage, consider using several repeated applications of the Hydro-CM program instead of the sodium phosphate or polyethylene glycol laxatives.
A. Why does surgery cause constipation?
The obligatory preparation for most surgeries, particularly abdominal, involves all the same steps and actions as for colonoscopies — a form of ambulatory surgical procedure.
To understand and appreciate why it takes so long and why it is so difficult to resume moving the bowels after these surgeries, factor in extended bed rest, general weakness, longer and more intense anesthesia, intense use of pain relievers after the surgery, and the widespread use of antibiotics to eliminate the post-surgical infection.
The recovery approach for post-surgical constipation is the same as described above for post-colonoscopy. Obviously, a high-fiber diet for a person recovering from surgery is akin to pouring acid onto an open wound. Unfortunately, that is what most doctors recommend. Not surprisingly, a lot of people survive perfectly-executed surgeries only to die later on from assorted complications, caused, in part or whole, by this terrible advice.
A. Why does hot weather cause constipation?
High temperature, especially when combined with dry air, causes rapid and insidious loss of body fluids and sodium with perspiration. To alleviate dehydration, the body removes moisture and sodium from digestive fluids and stools, turning them dry, hard, and difficult to move without pain.
When stools become small and dry, you aren't likely to experience the urge to move the bowels, making an already bad situation worse. In some instances, rapid dehydration may also cause diarrhea, which will further disrupt regular bowel movements. I explain the reasons behind this phenomenon here.
To prevent dehydration, keep yourself well hydrated in advance by drinking mineral (hard) water with added salt (1/2 to 1 teaspoon for each 250 ml glass), a solution known as isotonic or slightly hypertonic.
You should also drink it on an empty stomach, otherwise, the water will not reach the intestines quickly enough and when in excess, may cause vomiting. Do not drink too much and too quickly because you may stimulate precipitous urination and ensuing a loss of potassium, a mineral that is also needed for retaining moisture in stools.
If your stools are already hard and dry, avoid straining to prevent anorectal tear, abrasion, and ensuing blood loss. Instead, use the Hydro-CM program to break down and dissolve hard stools and to safely evacuate them. You may need several repeated applications to 'cleanse out' the bowels.
If stools remain hard and dry (type 1 on BSF scale) even after you are properly hydrated, it means there aren't enough bacteria in your gut to retain water in your stools. In this case, review the Restoring Intestinal Flora page, and use the Hydro-CM program to restore intestinal flora.
A. Can constipation cause acne?
No, not directly. Indirectly, however, constipation is one of the outcomes of a high-fiber diet that is behind elevated triglycerides — a high level of fatty acids in the blood. These fatty acids are formed by the liver from excess blood sugars (glucose, fructose, and glucose) and are further augmented by vegetable fats from dressings, fried food, and the like. In turn, blood sugars come from excess carbohydrates that accompany fiber, usually 5 to 10 times as many by weight.
Since young people can't yet efficiently deposit excessive triglycerides into the adipose (fat) tissue, these fats are being 'pushed out' through the sebaceous glands, making the facial skin fat and dry because excess fat blocks moisture.
When some of the sebaceous glands get clogged by excess fat, they provide a perfect breeding ground for trapped bacteria because some bacteria love to devour acidic fats. The ensuing eruption caused by the byproducts of bacterial fermentation becomes 'acne.'
So, why, then, do not all teenagers who are constipated develop acne, and why are not all who have acne constipated? Well, there are many other factors behind either constipation or acne. A high-fiber diet is only one commonality among all these factors.
Thus, reducing fiber and carbohydrate consumption may help relieve constipation by making stools smaller and eliminating acne by reducing elevated triglycerides. You should also pay attention to all other contributing factors, such as proper skin hygiene for acne, dysbacteriosis in the case of constipation, and so on.
A. What are the causes of constipation during pregnancy?
The uterus is located in the abdominal cavity along with tightly packed small and large intestines. As the uterus expands in size and weight, the outward pressure in all directions compresses the intestines and the stomach, and this pressure interferes with the mechanical aspect of gastric digestion (stomach's contraction and expansion) and the propulsion of chyme (digestive mass) through the intestines (motility).
Also, because the relentless pressure has a stimulating effect on the intestines, similar to the gastrocolic reflex, the peripheral nervous system adapts by suppressing it somewhat, so you end up missing bowel movements and making an already bad situation worse.
If you follow the standard medical advice regarding pregnancy-related constipation, and add more fiber and fluids into the mix, you'll accomplish the complete opposite effect — a constipation even more severe. Fiber is well known for causing obstructions in absolutely healthy adults. Just imagine how easily it can obstruct an already squeezed intestine during pregnancy.
Furthermore, fiber fermentation will cause even more interference with peristalsis and motility by causing acidity-related inflammation and ensuing bloating from trapped gases.
In general terms, women who become constipated during pregnancy have likely been affected by latent constipation prior to the pregnancy. Ideally, you should eliminate this condition before the pregnancy in order to prevent constipation from ruining one of life's most beautiful experiences, as well as preventing colorectal damage from straining and avoiding fetus damage from malnutrition caused by intestinal inflammation. To eliminate constipation prior to pregnancy, start here: No Downsize, Just Upside-down.
Since most medicinal laxatives are potentially teratogenic (may negatively affect fetus development), consider using the Hydro-CM program instead to keep stools small, moist, and easy to pass. Make sure to consult your doctor before using this or any other supplement, particularly during the first trimester.
A. Why does constipation cause enlarged internal hemorrhoids?
Hard stools, either large or small, are the hallmarks of functional, latent, and organic constipation and require straining while moving the bowels. The resulting inward pressure by hard stools on the hemorrhoidal pads that line the anal canal and the outward pressure from the abdominal and pelvic muscles to facilitate straining cause their enlargement for the same reason shoveling snow or paddling a boat with unprotected hands cause calluses on your palms.
I describe the sequence of events that precipitate hard stools and straining on this page: The Bull's S..t In the China Shop. Straining itself is the hallmark of latent (hidden) constipation, and there is only one way to eliminate it — by normalizing stools. I describe what's 'normal' and what's 'abnormal' on this page: What Exactly Are Normal Stools?
A. Why does constipation cause anal bleeding?
For the same reasons, hard stools cause enlarged internal hemorrhoids. They may also tear apart the delicate tissue that lines the rectum and anal canal. The resulting abrasions, fissures, ulcers, and fistulas may bleed when aggravated by straining. To eliminate bleeding and heal wounds, follow all of the recommendations below.
The Hydro-CM program is particularly useful for this purpose because it is safe for extended use, doesn't cause additional irritation, and non-addictive. It would help if you also eliminated all traces of fiber because fermentation increases the acidity of stools, and, in turn, it prevents the healing..
Since constipation and dysbacteriosis are concomitant conditions, it may also mean that you may be short on vitamin K — a blood coagulation factor — that is produced almost exclusively in vivo by intestinal bacteria. So, make sure to eliminate this condition as well by using the Hydro-CM program.
A. Why does constipation cause bloating and flatulence?
Bloating and flatulence are related to two concomitant conditions — intestinal inflammation and indigestible fiber fermentation by intestinal bacteria. Since constipation leads to a considerable accumulation of stools inside the large intestine, sometimes, even in the small intestine, bacteria have an infinite amount of undigested fiber to ferment on and produce copious gases and elevated acidity — the primary factor behind ensuing inflammation. In turn, inflammation blocks the absorption of gases into the bloodstream for evacuation through gas exchange in the lungs. These trapped gases cause flatulence and cramps, and the gases that gradually escape cause flatulence.
If you are affected by bloating and flatulence even without apparent constipation (i.e., not moving the bowels for more than three days), you may be affected by latent constipation— an abnormal accumulation of stools, even though your bowel movements are regular. I describe this condition at greater length here. There you'll also find treatment recommendations.
The worst approach to bloating and flatulence — constipation or not — is following the standard medical advice to consume more fiber, which is the equivalent of pouring a starter fluid over burning coals. When the situation becomes unbearable, instead of removing the fiber, doctors commonly prescribe antibiotics to wipe out any innate bacteria — an approach similar to treating migraine by butting your head against the wall until you drop down unconscious: no consciousness — no headache!
A. Why does constipation cause chronic fatigue?
In general terms, constipation is the tip of the iceberg in a long chain of digestive disorders, particularly malnutrition caused by fiber. If you doubt fiber's ability to cause malnutrition, ask yourself this question: Why do fiber supplements assist in weight loss?
The answer: it does by blocking the absorption of fats, of course. Alas, by blocking the absorption of fats, you also block the absorption of fat-soluble vitamins A, D, E, and K, and minerals, such as calcium and magnesium, because they depend on these vitamins for their assimilation. A deficiency of these minerals, in turn, causes circulation and muscle tissue problems that are partially behind chronic fatigue syndrome.
Here is another example: the fermentation of fiber and the rotting of undigested proteins produce toxic substances, such as methanol and cadaverine, that get assimilated into the blood and cause severe fatigue.
It would be best if you also investigated other malnutrition-related causes, such as non-iron dependent anemia, metabolic disorders, and thyroid dysfunction that are also connected to fat malabsorption.
These are just three examples. Eliminating fiber and constipation may help a great deal. Your doctor may help you diagnose and eliminate other problems, such as chronic infections, cardiovascular diseases, hypoglycemia, side effects of medicines, and numerous others.
A. Can constipation reduce my immunity?
Yes, absolutely. The intestinal flora is responsible for maintaining the non-specific primary immune response, or phagocytosis — a significant function of the immune system used to remove cell debris, viruses, bacteria, and cancerous cells. Since constipation is commonly associated with missing or damaged bacteria, you can pretty much add ‘one and one‘ to realize the impact of constipation on your immune system.
If you read most of this page, you must also realize that chronic constipation is also behind the toxins related to fermentation of carbohydrates, the rotting of proteins, and the inflammation of the bowels in different degrees of severity. Naturally, all three conditions depress and 'subdue' an already weakened immunity, leaving you more exposed to other pathogens.
Eliminating dysbacteriosis kills, figuratively speaking, a bunch of birds in one shot: protects the mucosal membrane of the large intestine from various pathogens, including cancer-causing; normalizes stools and relieves constipation, recharges primary immunity, resumes the synthesis of several essential vitamins, and eliminates the dependence on fiber to move the bowels.
You can learn more about the functions of intestinal flora on this page: Dysbacteriosis (Dysbiosis).
A. Can constipation cause bad mouth odor?
Yes, it can, but not in the ways you may think it does because there is a significant disconnect between the foul smell of stools and mouth odor.
In general, bad mouth odor, or halitosis, is caused by dental caries, periodontal disease, and sulfur-producing bacteria in the oral cavity. So, you must concentrate first on taking care of these conditions.
Here is where the connection takes place... Intestinal bacteria synthesize vitamin K, which is responsible for blood coagulation. When the said bacteria are missing, you are likely to experience gum bleeding, gingivitis, and periodontal disease. These three conditions precipitate inflammatory diseases affecting the tissues that surround and support the teeth, or periodontium.
As gingivitis progresses, subgingival (under the gum) bacteria colonize the inflamed periodontal pockets and cause progressive bone loss behind tooth loss in the long term. The byproducts of bacterial action cause a foul odor.
You can treat periodontal disease all you want. Still, it will not entirely go away until your restored intestinal flora starts producing vitamin K again to enable blood coagulation and healing.
Of course, this is only one aspect of preventing periodontal disease, tooth loss, and halitosis. Still, it is a big one, and here is your indirect connection to foul mouth odor.
The other connection is more insidious. Chronic constipation may result in a condition known as "fecal reflux" back into the small intestine. It happens when there is no room left in the large intestine to retain stools.
Unlike the large intestine, the small intestine can absorb smells in the bloodstream and carry them to the lungs for expulsion, hence the foul smell when you exhale.
Another rare condition that leads to the same outcome is the incomplete closing of the ileocecal valve -- a sphincter that separates the small intestine from the first section of the large intestine called the cecum (blind gut).
This defect allows the smells and gasses to escape into the small intestine with the same outcome as the reflux. To the best of my knowledge, I am the first person who has described these two conditions.
A. Is it true that old stools can cause "encrustation" of the large intestine‘s walls?
No, they can't, unless you are reading a deceptive advert for a 'colon cleanser' or 'colonic therapy.' It is pointless to enter into a debate with quacks and charlatans behind this gimmick, except to point out that you can't bind a 'crust' to the mucosal membrane inside the colon for the same reason that food can't form a crust inside your mouth.
A. What is the connection between constipation and appendicitis?
"Appendicitis is the sudden swelling and inflammation of the appendix. It generally follows the obstruction of the appendix by undigested food or a large accumulation of hardened stools (fecal impaction)." (Fiber Menace, page 32).
The accumulation of hardened stools in the cecum (blind gut, the location of the appendix) is one of the outcomes of latent constipation. In healthy adults, the contents of the cecum are liquid or semi-liquid but never solidified.
A. What is the connection between constipation and colorectal cancer?
Quite direct: Large and heavy stools cause polyposis and flat lesions throughout the entire length of the colon. Some polyps and lesions turn cancerous, particularly in people with reduced immunity, also precipitated by constipation.
I address this connection at length on this page — Colon Cancer Prevention Guide: Step 1. Normalize Abnormal Stools.
A. Why doctors aren‘t recommending a recovery protocol similar to your Hydro-CM program?
Many do, particularly in countries that provide universal health care, such as Germany or Russia. Bacterial therapy is the most common treatment approach there for functional colorectal disorders discussed on this page.
Unfortunately, not so in the United States because in cases of colorectal complaints, the U.S.-based doctors invariably are looking for ulcers, polyps, inflammation, bleeding, enlarged hemorrhoids, and so on. When these late-stage pathologies aren‘t found (as is usually the case), the patients‘ conditions are considered idiopathic (of unknown origins) or psychosomatic ("in your crazy mind").
It wouldn‘t happen, of course, if physicians examined stools and checked the status of intestinal flora — the two major determinants of colorectal health. But beyond the perfunctory, fecal occult blood check, physicians in the U.S. (1) rarely examine stools; (2) intestinal flora isn‘t considered essential, and (3) dysbacteriosis isn‘t recognized as a bona fide disorder. More...
A. What are the most common side-effects of traditional laxatives?
Please review the following links to get a complete picture:
— Agents Used To Treat Constipation (The Merck Manual of Diagnosis and Therapy);
— Loosening up hard stools (Overcoming Fiber Dependence)';
— To avoid side effects and to improve the outcomes of treating constipation, I recommend using the Hydro-CM program. The following table enumerates its safety vis-à-vis other methods: the Hydro-CM Program Safety vs. Common Laxatives
While preparing this page for publication, I came across an article about constipation on the web site of The International Foundation for Functional Gastrointestinal Disorders (IFFGD), which I quoted in Fiber Menace all the way back in 2005. Here is their new tune regarding dietary fiber:
"Dietary fiber is often effective in improving mild constipation. However, it has less consistent results with more severe constipation, possibly worsening symptoms in patients with slow colonic transit (colonic inertia) [12]"
Despite the good beginning, the rest of IFFGD's site still recommends fiber to relieve and prevent constipation—though only for healthy people this time around. That's one good way to become unhealthy and turn "mild" constipation into "severe."
No surprise there — Procter & Gamble, the maker of Metamucil, is one of IFFGD‘s corporate sponsors [link], so IFFGD is already "covering its bases" with a skillfully worded disclaimer to absolve itself from future culpability. When there is a choice between making a buck and making people healthy, the buck wins..
Please don't forget to send a link to this page to anyone you know, suspect, or believe may be affected by constipation. For all the work I do, nothing elicits as much happiness and joy among my readers as being able to go to the bathroom without a fear. Make someone happy and joyful again!
Konstantin Monastyrsky
Thank you! I have just purchased your book and am trying two of your products. I cannot believe how much hype I have swallowed over the years. It has only been a week; I have lost 7# by doing almost nothing and already feel SO much better—a healthier end is now in sight!!!" G.R., USA (via e-mail)
Footnotes
You can click the Backspace key on your keyboard or the browser's Go back button to return to the referring text.
Click the [link] to view the source site or document in the new window (when available). The references for this guide were compiled in early 2008. Some of the links may not match at a later date because publishers may revise their web sites. In this case, try searching cached pages on Google, or contact the respective publishers.
1 Constipation; The Merck Manual of Diagnosis and Therapy; 18th edition; on-line version [link]
2 Epidemiology of constipation in the United States. Sonnenberg A. Koch TR., Dis Colon Rectum. 1989 Jan;32(1):1–8.
3 R. Jensen, D. Buffangelx, G. Covl, CLINICAL CHEMISTRY, Vol. 22,No.8,1976 1351
4 Stool Analysis; Digestive Disorders Health Center; WebMd.com [link]
5 Malabsorption Syndromes; The Merck Manual of Diagnosis and Therapy; on-line edition [link]
6 International Space Station Integrated Medical Group (IMG) Medical Operations Book All Expedition Flights, Mission Operations Directorate, Operations Division, JSC-48511-E1, 24 August 2000 [link]
7 R. Jensen, D. Buffangelx, G. Covl, CLINICAL CHEMISTRY, Vol. 22,No.8,1976 1351,
8 Position of the American Dietetic Association: Health Implications of dietary fiber; Journal of The American Dietetic Association; July 2002; Volume 102; Number 7, page 995
9 Rome II: The Functional Gastrointestinal
Disorders;
C29.7:731; by Douglas A. Drossman (editor);
10 R.F. Schmidt, G. Thews. Colonic Motility. Human Physiology, 2nd edition. 29.7:731.
11 What are the side effects of statins; MedicineNet.com (a service of WebMD); [link]
12 Dietary Fiber; International Foundation for Functional Gastrointestinal Disorders [link]